
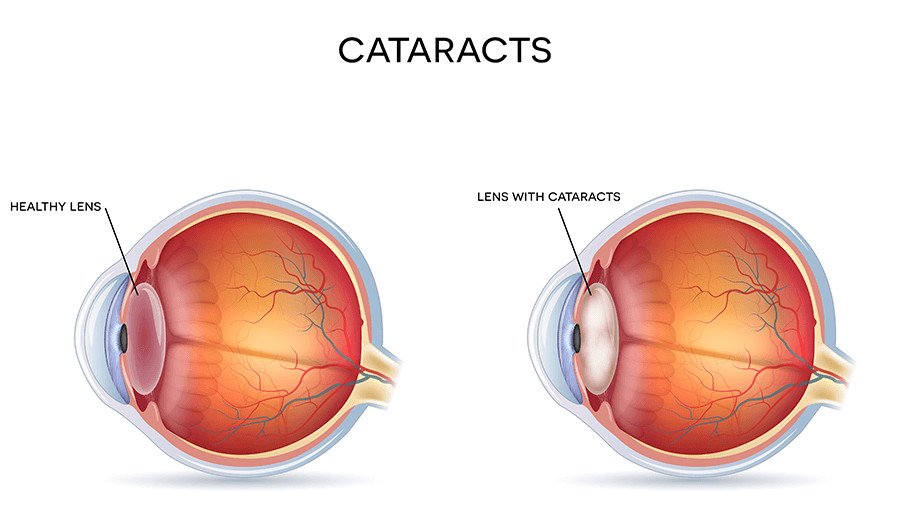
Cataracts occur when the natural lens of your eye becomes cloudy, causing blurry vision and other visual symptoms. This common age-related condition affects millions of people each year and is a leading cause of vision impairment.
When you have cataracts, it’s like looking through a foggy window. Colors may appear faded, night vision becomes poor, and everyday activities like reading or driving become increasingly difficult. Cataracts develop gradually, so many people don’t realize they have them until vision is significantly affected.
The good news? Cataract surgery is one of the most successful and commonly performed procedures in the United States, with a high safety profile and excellent outcomes.
Nearly 24.5 million Americans have cataracts, which is a leading cause of blindness, according to the American Academy of Ophthalmology.
Your eye’s natural lens must be clear for the retina to receive a sharp image. If you have cataracts, your eye’s natural lens becomes cloudy, making it difficult to perform simple tasks such as reading a book or seeing road signs clearly.
During cataract surgery at our Jupiter, FL location, Dr. Benaim, our expert ophthalmologist, removes your eye’s clouded natural lens and replaces it with a clear, artificial intraocular lens (IOL). With more than 20,000 successful cataract surgeries performed, Dr. Benaim provides Jupiter residents with exceptional eye care you can trust.
If you’re experiencing blurred vision or any cataract symptoms, schedule an appointment at our Jupiter, FL, office today to restore your clear vision.
You may need cataract surgery if your vision has deteriorated to the point where it interferes with your daily activities and quality of life. Typically, candidates for cataract surgery include:
The only effective treatment for cataracts is to surgically remove the clouded lens and replace it with a clear artificial one.
If Dr. Benaim determines you need cataract surgery, he will guide you through the process and answer all your questions. Dr. Benaim will also help you select the appropriate intraocular lens (IOL) to replace your clouded natural lens.
He’ll consider your current prescription, lifestyle needs, and whether you have astigmatism before recommending the best permanent lens option available in Jupiter, FL. Our team will work with you to schedule surgery at a time that best accommodates your needs.
Dr. Benaim begins the procedure by applying eye drops to dilate your pupil and numb your eye with a gentle topical anesthetic for your comfort. Then, he will make a small incision and insert a tiny ultrasonic device.
The front part of the lens envelope, known as the lens capsule, is carefully opened, and the hardened, yellowed proteins forming the cataract will be broken up into tiny pieces and removed. The clear artificial lens selected by you and Dr. Benaim is then inserted through the original incision and centered within the lens capsule.
The lens will remain securely positioned within your eye. Intraocular lenses cannot be felt or sensed in any way. Dr. Benaim ensures proper lens positioning, and the incision typically self-seals without requiring stitches.
The surgery is generally an outpatient procedure at our Jupiter location, lasting only about 10 to 15 minutes.
Recovery after cataract surgery at Benaim Eye is typically quick, with some patients seeing improvement in as little as 24 hours. You will receive eye drop medications to be administered several times daily for the first few weeks following surgery.
You can also expect to see Dr. Benaim for a few follow-up appointments to ensure your eyes are healing well and your vision is improving. It is important to follow any and all instructions provided to you to reduce the chance of complications.
Most patients achieve noticeably better vision within the first 24 hours after their procedure. Following your return home, Dr. Benaim often personally calls to check on your progress.
Our team will schedule a follow-up appointment to ensure optimal healing, clear vision, and that you’re enjoying seeing the world through your “new” eyes. Many patients experience significantly improved color perception and night vision after surgery, along with reduced dependence on glasses for certain activities.
However, for some people, it can take a few weeks for their eyes to adjust to the new lenses and for their vision to reach its full potential.

At Benaim Eye & Aesthetics, we specialize in restoring vision and enhancing quality of life through expert cataract care. Utilizing cutting-edge technology, we provide precise diagnosis and advanced treatments to address cataracts, helping you experience the world with renewed sharpness and vitality.
Cataract surgery is typically an outpatient procedure, lasting about 10 to 15 minutes. The recovery period after cataract surgery is also pretty short. Some patients recover as quickly as 24 hours. Most patients achieve noticeably better vision within the first 24 hours of the procedure. Dr. Benaim has performed more than 20,000 cataract removal surgeries, so you can rest-assured that you’re in good hands.
You don’t have to take our word for it though. Hear directly from our cataract surgery patients, who are loving their new found ability to see the world clearly.
Accordion Content
Cataracts develop due to various factors:
Understanding these causes can help you protect your vision as you age.
Cataracts often develop gradually, but as they progress, you may experience:
If you notice these symptoms, it’s time to schedule an evaluation with Dr. Benaim.
Diagnosing cataracts at Dr. Benaim’s office is a comfortable and straightforward process. We use the following tests:
These painless tests help us determine if cataracts are affecting your vision and guide us in creating a treatment plan tailored to you.
The outlook for cataract patients at Benaim Eye & Aesthetics is highly positive. Here’s why:
At Dr. Benaim’s office, we are committed to helping you achieve and maintain clear, comfortable vision through compassionate and personalized care.
The first sign of cataracts is often blurry or cloudy vision, which can gradually worsen over time. Other early signs may include increased sensitivity to glare, difficulty seeing in dim light and seeing halos around lights, especially at night. If you experience any changes in your vision, it is essential to schedule an eye examination with the experts at Benaim Eye and Aesthetics for a comprehensive evaluation and diagnosis.
The three primary types of cataracts are nuclear cataracts, cortical cataracts and posterior subcapsular cataracts. Nuclear cataracts form in the center (nucleus) of the lens, cortical cataracts develop in the lens cortex and posterior subcapsular cataracts occur at the back of the lens capsule. Each type of cataract may present with different symptoms and require specific treatment approaches, which can be discussed with the experienced team at Benaim Eye and Aesthetics.
While there is no proven way to prevent cataracts from forming or progressing, certain lifestyle modifications may help reduce the risk or slow the progression of cataracts. These include wearing sunglasses with UV protection, eating a balanced diet rich in antioxidants and nutrients, quitting smoking, managing underlying health conditions such as diabetes, and attending regular eye examinations for early detection and treatment.
The primary cause of cataracts is age-related changes in the eye’s natural lens, leading to the accumulation of protein clumps and cloudiness. Other factors such as prolonged exposure to UV radiation, smoking, diabetes, eye injuries and certain medications can also increase the risk of developing cataracts. Understanding and addressing these risk factors, along with regular eye examinations, can help reduce the risk of cataracts and preserve vision.
Cataracts are a common eye condition that can significantly impact vision and quality of life if left untreated. While cataracts themselves are not usually considered serious or life-threatening, they can lead to significant vision impairment and interfere with daily activities such as reading, driving or recognizing faces. Early diagnosis and treatment are crucial for effectively managing cataracts and preserving vision.
Cataracts can worsen suddenly as a result of various factors such as increased exposure to UV radiation, eye trauma or injury, certain medications and underlying health conditions such as diabetes or high blood pressure. Additionally, changes in lifestyle habits such as smoking or poor nutrition may also contribute to the progression of cataracts. It’s essential to attend regular eye examinations to monitor changes in vision and detect any worsening of cataracts.
While cataract surgery remains the gold standard treatment for advanced cataracts, researchers are continually exploring new treatment options to improve outcomes and patient satisfaction. One promising approach is the use of femtosecond laser technology to perform cataract surgery, which offers greater precision and customization compared to traditional surgical techniques. Additionally, advancements in intraocular lens technology, such as multifocal and extended depth of focus lenses, aim to provide improved vision outcomes and reduced dependency on glasses following cataract surgery.
In the early stages, cataracts may not cause significant symptoms or visual disturbances, making them difficult to detect without a comprehensive eye examination. However, some early signs of cataracts may include mild blurriness or cloudiness in vision, increased sensitivity to glare and difficulty seeing in dim light. If you experience any changes in your vision, it is essential to schedule an eye examination with the experts at Benaim Eye and Aesthetics for a comprehensive evaluation and diagnosis.
While there is no proven way to clear cataracts without surgery, certain lifestyle modifications and protective measures may help slow their progression and alleviate symptoms. These include wearing sunglasses with UV protection, eating a balanced diet rich in antioxidants and nutrients, quitting smoking, managing underlying health conditions such as diabetes, and attending regular eye examinations for early detection and treatment.
Blindness after cataract surgery is rare but can occur as a result of complications such as infection, inflammation, retinal detachment or damage to the optic nerve. It’s essential to follow all post-operative instructions provided by your surgeon and attend all scheduled follow-up appointments to monitor your healing and address any concerns promptly.
The degree of vision improvement following cataract surgery depends on various factors, including the severity of cataracts, the individual’s overall eye health and the type of intraocular lens (IOL) implanted during the procedure. While most patients experience significant improvements in vision and quality of life following cataract surgery, some may still require glasses or contact lenses for certain activities such as reading or driving. The experienced team at Benaim Eye and Aesthetics will evaluate your condition and discuss the expected outcomes and treatment options tailored to your needs.
Once cataracts are surgically removed, they cannot regrow. However, some patients may develop a condition known as posterior capsular opacification (PCO), where the thin membrane behind the implanted intraocular lens (IOL) becomes cloudy over time, leading to visual disturbances similar to cataracts. PCO can be easily treated with a quick and painless laser procedure called YAG laser capsulotomy, which creates a small opening in the cloudy membrane to restore clear vision. Some ophthalmologists have a YAG laser in their office, making it unnecessary to return to a surgery center for this procedure.
While there is no proven way to stop cataracts from progressing, certain lifestyle modifications and protective measures may help slow their progression. These include wearing sunglasses with UV protection, eating a balanced diet rich in antioxidants and nutrients, quitting smoking, managing underlying health conditions such as diabetes, and attending regular eye examinations for early detection and treatment.
Certain medications, such as corticosteroids, antipsychotics and medications used to treat high blood pressure or cholesterol, may increase the risk of developing or worsening cataracts. It’s essential to discuss any medications you are taking during your eye examination to evaluate their potential impact on your eye health and vision.
Cataract surgery is typically not painful, as it is performed under local anesthesia to numb the eye and surrounding tissues. Most patients report feeling little to no discomfort during the procedure, which is performed on an outpatient basis. After surgery, some mild discomfort or irritation may occur, but this can usually be managed with over-the-counter pain relievers and prescription eye drops. The experienced team at Benaim Eye and Aesthetics will ensure your comfort and safety throughout the surgical process.
The decision to remove cataracts depends on various factors, including the severity of symptoms, the impact on daily activities and the individual’s overall eye health. In general, cataract surgery may be recommended when cataracts significantly impair vision and interfere with daily tasks such as reading, driving or recognizing faces. The experienced team at Benaim Eye and Aesthetics will evaluate your condition and recommend the most appropriate treatment approach for your needs.
While cataract surgery is generally safe and effective, like any surgical procedure, it carries certain risks and potential complications. These may include infection, inflammation, bleeding, swelling, retinal detachment and changes in vision. However, with advancements in surgical techniques and
technology, the risk of complications is minimal, and most patients experience significant improvements in vision and quality of life following cataract surgery.
Cataract surgery is typically performed when cataracts significantly impair vision and interfere with daily activities, regardless of age. While cataracts commonly affect older adults, surgery may be recommended at any age, depending on the severity of symptoms and the individual’s overall eye health.
With cataracts, vision may appear blurry, cloudy or distorted, similar to looking through a foggy or frosted window. Patients may also experience increased sensitivity to glare, halos around lights, and difficulty seeing in dim light or at night. As cataracts progress, vision may continue to deteriorate, making it challenging to perform daily activities such as reading, driving or recognizing faces. If you experience any changes in your vision, it is essential to schedule an eye examination for a comprehensive evaluation and diagnosis.
Cataracts may worsen gradually over time, leading to progressive blurriness, cloudiness or distortion of vision. Other signs that cataracts are getting worse may include glare, difficulty seeing in dim light or at night and seeing halos around lights. If you notice any changes in your vision, it is crucial to schedule an eye examination for a comprehensive evaluation and diagnosis to determine the severity of your condition and discuss treatment options tailored to your needs with the experts at Benaim Eye and Aesthetics.
Some studies suggest that certain medications used to treat high blood pressure, such as thiazide diuretics and beta-blockers, may increase the risk of developing cataracts. However, the link between blood pressure medications and cataracts is not entirely clear, and further research is needed to understand the relationship fully. It’s essential to discuss any medications you are taking, including blood pressure medications, with the experts at Benaim Eye and Aesthetics, during your eye examination to evaluate their potential impact on your eye health and vision.
High blood pressure, also known as hypertension, is a risk factor for various eye conditions, including cataracts. Chronic hypertension can affect blood flow to the eyes, leading to damage to the tiny blood vessels in the retina and increasing the risk of developing cataracts. Additionally, certain medications used to treat high blood pressure may also increase the risk of cataracts. It’s essential to manage blood pressure effectively through lifestyle modifications and medication under the guidance of a healthcare professional in order to reduce the risk of cataracts and other eye-related complications.
Using eye drops may help alleviate symptoms such as dryness, irritation or discomfort associated with cataracts, but they will not treat or cure the underlying condition. It’s essential to use eye drops as directed by your ophthalmologist at Benaim Eye and Aesthetics to avoid any drops that may contain ingredients that could exacerbate cataract symptoms or interfere with other treatments.
HOURS
Monday – Friday
8:30am-4:30pm
Closed Saturday & Sunday
Tel: 561-747-7777
Fax: 561-575-1921
info@benaimeye.com